southcentral
New Scrubs:

We started an incredible journey together. You were brand new and I was a brand new face to staff and residents. We showed up together, ready to make a difference and bring some smiles and relief to those in need. We were new, wrinkle free and ready to go…fresh, clean!
That first night, we met so many new faces and saw so many different scrubs; all in different phases of use and wear. We stood out…too new, unwrinkled, unsure of ourselves, too clean, we stood out. We saw so many things in everyone’s eyes….fear, exhaustion, desperation, concern, defeat, compassion. That first night we learned so much together, brought many smiles to new faces, watched as people milled about and doing their thing. We quickly became dirty ourselves yet still had that nice crisp look to us. We did our best to learn, to fit in.
We came back to our room after that first night; exhausted and ready for a break. We washed the night away with soap and water, we thought about what was to come. As the nights went on we, ourselves became wrinkled, dirty, worn. No matter how well we took care of ourselves…we couldn’t remove the wrinkles like we did so many times to remove the wrinkles on the beds the residents laid upon.
We watched as residents went from being able to move around on their own and take care of their own basic needs to being bed ridden and helpless. We tried in vain, to remove the wrinkles from these beds to make it more comfortable for them, just as I tried to remove the wrinkles from you. Then I realized that wrinkles weren’t so bad. Your wrinkles showed you care, you are there for these people and we are all in this together….we are bonded, we are wrinkled. We watched in horror as more and more continued to spiral downward. We sat on the beds of so many, holding their hands, washing them with soap and water and telling them they are loved. We were the last voices some heard, the last touch they felt, the last loving words they would hear, the last person to say “I love you”. We, us…..me and my wrinkled scrubs. We quickly became part of this family; all of us wrinkled, dirty, tired and compassionate….together.
As the exhausting nights went on we became more and more weary of returning to work as we were never confronted with good news. We held coworkers as they mourned the loss of another resident. We secretly cried when we got home because we had become so attached to these new faces, these wonderful people. We secretly sat every morning and reflected on the night before and wished these wrinkles would just go away. We get to work one day, feeling defeated and are met with the best news, residents are starting to get better! We sat with these very sick and undefeated residents and held their hands….you are loved, you can fight this, you are too strong to give up…..don’t ever give up!
As I was carefully folding you, trying to get the wrinkles out and putting you away I realized; we too have become warn, scared, exhausted, defeated but our compassion and determination has never wavered. We miss our family and our home greatly but we must continue to carry on with what I signed us up for. You took care of me, protected me as I protected you, washed you and cared for you as we both did for our residents. Our last night was different; we saw the beginning of something horrible and went through the worst times with all the other pairs of scrubs and finally through days/nights getting easier.
Together we all made it through this storm, wrinkled, worn and tattered but still standing tall. We quickly realized how amazing the women and men wearing these other scrubs truly are. With minimal resources at our disposal we were able to bring people back from near death….what an amazing feeling. How proud we feel for the others wearing these scrubs. We forged new friendships, new memories with the others wearing the scrubs and residents alike. We went from being so concerned and constantly on our feet caring for these people to being able to just watch them sleep and rest. We sang with the women in the other scrubs and danced in the hallways as our wonderful residents slept and regained their strength. We danced with joy because these residents made it! We danced to honor those that didn’t survive yet still brought joy to our lives just days and hours before they passed, because they were now free of their pain. We danced because we all weathered this storm together. Our scrubs now equally worn, tattered, wrinkled and dirty have seen the worst and best with us and now dance with us. We sang and danced because we finally had a chance to look at the positives and not continue on with negatives. As I fold you for the last time, so neatly, I realize I am putting away another chapter in our lives. We are thankful for our team and family and these, oh so beautiful, wrinkles. We are thankful for those that fought so hard and said, not today God, not today…….
Jaimie Adams, South Central/Seacoast MRC Volunteer, Firefighter/EMT
Workplace Mental Health
Maintaining employment can be difficult if you are living with depression or a mood disorder. Despite the desire to have regular and stable income, to be productive and to enjoy the structure of routine, working with depression or a mood disorder can be challenging because of the stressful demands that employment can bring.
Depression is currently the number one cause of disability in the world according to the World Health Organization (WHO). For those who suffer with depression, managing stress and potential triggers in the workplace can be difficult. This is an issue that both employers and employees need to address together.
Tips for the employee:
- Have your self-care arsenal ready to go: Whether it’s the weekly yoga class or spending time with your family, try to find some way to unwind after a long day. It’s a great way to keep your mental health in check.
- Make sure you are getting enough sleep!
- Keep your medical team in the know: Your doctor, your psychiatrist, and other medical professionals are on your side and want to see you succeed. Keep them in the loop on how you’re feeling.
- Prioritize and strategize: You can’t do it all. Prioritize the most important tasks and make a strategy on how they should be tackled.
- Put yourself first: You can’t do it all. Learning to say no and putting yourself first is difficult but critically important for your mental health.
Employers and business owners should consider the work environment as well. The WHO estimates that depression costs the global economy over a trillion dollars a year. This is due to absenteeism and lost productivity. Helping your employees is not only the right thing to do but it can help the bottom line.
Tips for employers:
- Ensure a safe work environment: Hazards can cause stress if an employee is always worried about getting hurt on the job.
- Be aware of work/life balance: Keeping an employee at work for more than 8 hours eats in to their time with their family and friends. It’s hard to practice self-care when there’s only so many hours in a day.
- Set realistic expectations and goals: Base these goals on the employee’s skill set. Everyone is good at something but not everything. Help them find their niche within the business where they can thrive.
- Compensate fairly: A living wage is so important when it comes to stress. If an individual is not making enough to cover living expenses it causes a lot of stress. Not only will the employee probably not stay with the company for long but they could be constantly distracted while on the job.
- Bonus: Recognize the mental health day!
Depression is a common, manageable disease. No one can tackle it alone, especially when it comes to maintaining employment. When employees and employers work together to tackle this issue, we all win.
Other resources:
http://workplacementalhealth.org/Mental-Health-Topics/Workplace-Stress
https://www.who.int/mental_health/in_the_workplace/en/
Christmas Tree Transportation Safety
Christmas Tree Transport Safety
How many tree-topped vehicles will you spy this month? The Christmas tree buying season is in full swing! Before you leave your home to find that perfect tree, measure the dimensions (height, width, depth) of the expected trees location in your home to make sure that the perfect Christmas tree fits in your space!
The American Automobile Association (AAA) offers some tips for transporting trees:
Make sure to bring strong rope or nylon ratchet straps, an old blanket, gloves and of course – the right vehicle. One with a roof rack is ideal but a pickup truck, SUV, van or minivan can work just as well.
Have the lot wrap the tree in netting before loading it. Loose branches can also be secured with rope or twine to help protect the tree from damage.
Cover the roof with an old blanket to protect the car from any damage.
Place the tree on the roof rack or in the bed of the truck with the trunk facing the front of the car. If the vehicle does not have a roof rack and is large enough – place the tree inside.
Secure the tree at its bottom, center and top using strong rope or nylon ratchet straps. Avoid using the twine offered by many tree lots. Use fixed vehicle tie-down points and loop the rope or strap around the tree trunk above a branch to prevent any side-to-side or front-to-rear movement.
Once tied down, give the tree several strong tugs from various angles to make sure it is secured in place and will not come loose.
Drive slowly and take back roads if possible. Higher speeds can create significant airflow that can damage your tree or challenge even the best tie-down methods.
Wishing you Safe Travels and a Happy and Healthy Holiday Season!
Storing Medications While Traveling
Over the holidays many people will be traveling. Regardless of what holiday you celebrate and when, you may need to travel in order to be closer to friends and family members. Flights are booked, accommodations are made, pet sitters have been found but how do you manage your medications while away?
- In a car: Keep all the medication in its original containers and put it in your luggage bag. Medication should be kept away from extreme temperatures such as the heating vent in your car or the cold of the trunk. This means keeping out of the glove compartment, the center console, the trunk, and away from the floor board in the front seat. It’s best to keep it in the back, away from vents (Consumersafety.org).
- On a plane: Keep all medication in its original containers and store it in your carry-on bag (just in case). Have a list of your medications and why you take them with you in case TSA asks for it. Then the bag is cleared to fly, this also keeps the medication from being subjected to extreme cold in the cargo storage (safemedication.com).
Some other things that need to be considered:
- When storing medications at the destination keep them in the original containers, especially if you’re traveling with children. If you have access to a safe or a safe storage container, that should be used as well when traveling with other people (upandaway.com).
- Does this medication need to be refrigerated? Things like Insulin need to be kept cool even while traveling. Special medication cooler bags are available but a lunch bag with a frozen ice pack will work, too. However, keep the medication from directly touching the ice pack. The cooler can go through TSA as well but they will need to check everything inside of it and it might take a little time. Any IV bags, pumps, or syringes will need to be inspected and the liquids are likely to be as well. Having a signed slip from your doctor would be helpful during this time (safemedication.com).
- What about time zones? If you’re traveling further away through a time zone change, talk to your doctor or pharmacist about taking your medications. They will be helpful in developing an action plan so just the right amount is being taken at the correct time (consumersafety.org).
- Lastly, while traveling it’s easy to forget when to take a medication. Setting an alarm on a phone or watch could be a helpful reminder (consumersafety.org).
Additional resources to look at include:
Mental Health in The New Year
Resolve to Be Healthy: Mind and Body
People make lots of resolutions at the start of the New Year. We have heard them all: go to the gym every day; lose weight; improve our eating habits or drink less alcohol. They are all excellent goals but are very broad and can set up an individual to feel worse than better if they fall short. Focusing on physical well-being is very common. Emotional health is just as important. Working towards achieving balance in physical and emotional health is an excellent target for 2019. Take the time to stop ask yourself if you are too hard on yourself, rush through the moments in your life, miss time with family and friends or hibernate with singular focus on tasks and responsibilities.
Below are some ways to think about helping yourself feel more relaxed, supported and happy in your daily life. Just like any other resolution, these activities require some commitment and focus. See if you can picture yourself making some small changes to positively impact your life.
- LET GO OF PERFECTION: Setting a goal of being perfect can lead to acute disappointment. Mistakes are normal. Forgiving oneself for falling short of your own, other’s or society’s expectations is hard but very important to avoid a toxic level of perfectionism that can lead to emotional issues like anxiety, depression, or more serious things. Don’t be afraid to ask for help if you recognize this trait in yourself. https://www.medicalnewstoday.com/articles/323323.php
- BE MORE PRESENT: If you spend every day thinking about what you need to do or what you want for tomorrow and the future, you may miss a moment in the time you are in that makes you happy or helps you to feel content. Try to appreciate the place you are in and the people you are with. There is nothing wrong with setting goals and planning for the future, but if you focus solely on that you may miss a moment or encounter in the present that would make you smile and feel good. This is a part of learning to be mindful. Practicing mindfulness takes practice. Some people choose meditation, deep breathing, walking, yoga or a host of other calming activities to help them achieve it. https://www.psychologytoday.com/us/blog/when-your-adult-child-breaks-your-heart/201801/five-new-year-s-resolutions-improve-your-mental

- SPEND TIME WITH FRIENDS AND FAMILY: Isolation can be very harmful to an individual. Certainly it is fine to want to spend time alone but being alone without regular contact with others can be damaging to your emotional heath and lead to depression, anxiety, low self-esteem and other issues. Spending time with family and friends can be very nourishing. Though potentially hard to initiate, making the effort to reconnect with friends and family can pay off in a very significant way. Greet your New Year and phone a friend. Here are some tips of navigating the process: https://www.psychologytoday.com/us/blog/the-man-cave/201808/5-proven-steps-reconnect-family-and-friends
- SELF-CARE: Make an effort to turn off and tune out from social media and relax. Find some time every day to do something that makes you happy. Walk your dog, take a class, go for a walk alone, soak in the tub or sit quietly and read for 10 minutes. Find something to add into your routine that can give you that special “me time”. https://www.psychologytoday.com/us/blog/when-your-adult-child-breaks-your-heart/201801/five-new-year-s-resolutions-improve-your-mental

- GO OUTSIDE AND GET SOME FRESH AIR: Take the time to appreciate nature. Take a walk around the block. It can be as simple as seeing a blooming tree next to your bus stop and coming to appreciate its’ presence every day when you get there. Perhaps a small bird sits outside your office window and you look forward to seeing it. It is important to your emotional health to find a way to see things outside of your daily life and feel good about them. https://www.psychologytoday.com/us/blog/the-new-resilience/201801/why-connecting-nature-elevates-your-mental-health
 BONUS TIP: Adopt a couple of small plants. Place them on your windowsill. Care for them and watch them grow. You will be surprised at the improvement in your mood when you find yourself caring for a living thing. You may have an awesome green thumb!
BONUS TIP: Adopt a couple of small plants. Place them on your windowsill. Care for them and watch them grow. You will be surprised at the improvement in your mood when you find yourself caring for a living thing. You may have an awesome green thumb!
While making your resolutions for this New Year don’t forget your brain and your emotional health. Taking small steps to improve your mental health can help reduce your risk for many physical problems like heart disease and muscle soreness.
Mental Health Days
Mental Health Days
The stigma associated with accessing mental health and substance misuse services has been discussed in previous posts. Another stigmatized topic is the Mental Health Day. In our society and in particular, in the workplace mental health and physical health are not viewed in the same way. If someone is sick with the flu, we push them to stay home and rest so they can get better (and so they don’t spread germs). We know the event can be prolonged if the person returns to work while they are still ill. Why don’t we treat mental health the same way? When we acknowledge that Mental Health Days are valid, we will see improved attitudes in home and the workplace. Employers may experience improved productivity and decreased time out of work in the long term.
https://www.communityreachcenter.org/blog/take-mental-health-day/
How do I know if I need a Mental Health Day?
- You can’t focus on the smallest things or feel extremely distracted
- Because of that lack of focus, you’re beginning to feel more of a hindrance to those you meet than a help
- You’re exhausted but you can’t sleep from the thoughts of dreading work the next day
- You’ve noticed that it does not take much make you have feelings of anger or irritability
- You feel like you’re in a haze or moving in slow motion
When one of your coworkers misses work it might be flu, back injury, a dental procedure or a general problem such as low grade fever, headache or stomach disturbance. Both of you are experiencing symptoms that will interfere with your ability to do your job, interact with others and be productive over the course of the day. The symptoms may last longer than one day.
Many employers require a note from a physician or clinic when an employee misses more than two days of work. This is actually a good policy. If someone is feeling so unwell that they have to miss more than two consecutive days of work it is not unreasonable to ask them to be seen by a professional. In some cases, that requirement is the way in which employees uncover an undiagnosed physical or mental condition that requires treatment.
How what should I approach my employer if I need a Mental Health Day?
- It is unrealistic to predict when a person is going to feel overwhelmed or unwell.
- Follow the established guidelines of your employer for notifying them of your need to be away from work.
- If your work environment is positive and supportive, try to be as honest as possible with your employer.
- Otherwise, just report that something urgent has come up and you will be out.
- Some people with an ongoing need to have breaks, plan scheduled days of vacation off periodically to minimize other time out of work they might need.
It would be wonderful if all employers supported employee efforts to take care of their mental health. Workforce mental health is important not just to individuals, but to employers. The Center for Prevention and Health estimates mental illness and substance abuse issues cost employers as much as $105 billion annually. Reduced productivity, absenteeism, and increased health-care costs are just a few of the ways mental health issues cost employers money.
Taking a Mental Health Day periodically may help you to build mental strength and more agility when managing the stressors in your life.
Stigma and Treatment
The Substance Abuse and Mental Health Services Administration (SAMHSA) reports that 1 in 5 Americans will have some sort of behavioral or mental health disorder (MHD) at some point in their life. According to the National Institute of Health (NIH) 10% of Americans will have a substance misuse disorder (SUD) at some point in their life.
You may read that and think, “That’s not so many”. Consider this: Of the 20% of Americans who suffer with a mental health disorder, less than half will receive treatment. In addition, 76% of young people who suffer with depression receive no treatment for their condition.
(http://www.mentalhealthamerica.net/issues/state-mental-health-america).
Now is the time for change. Need for mental health and substance abuse treatment is increasing. Not all who need care are successfully accessing it.
A number of barriers exist to accessing care.
- Lack of professionals in both mental health and substance abuse.
- The cost of care – especially for those without adequate coverage.
- Stigma – defined as,” a set of negative and often unfair beliefs that a society or group of people have about something.” An individual deeply perceives a feeling of stigma in the cases of substance abuse and mental health disorders and is less likely to try to find care.
- Lack of Professional Development in Medicine– Even today many physicians, nurses and other health care professional are uncomfortable having a discussion with a patient about these issues. Professional development opportunities are lacking.
Read more about addiction and stigma:
https://drugabuse.com/library/addiction-stigma/
When someone is suffering from one of these conditions there are a few things to remember when interacting with them and encouraging them to stake steps towards improved well-being:
- Listen without judgement if someone confides in you
- Don’t use dehumanizing terms such as “Junkie”
- Research how drug dependency works and learn more about SUD/MHD
- Educate others on your findings
- Speak up when you see stigma
- Remember that anyone can fall victim to these conditions. Listen to the entire story.
- Remind the person that after they have completed treatment they have the potential to do anything they set their minds to.
- Be kind
Make other people matter in your life. Spread the word. Be part of the change. Make a difference. Choose wellness.
Your Brain and Addiction
When Richard Nixon declared a “War on Drugs” in 1971, no one anticipated that it would be one of the longest running wars in history and continue today. In 1987, the Partnership for a Drug Free American launched its “This is your brain on drugs” campaign, illustrating the rapid frying of a cracked egg in a hot pan.

The brain does change when you use substances. The human brain is the most complex organ in your body. It controls all human activity and intellect. Drug use will affect the way your brain functions and your behavior in a significant way.
When you engage in an activity that you enjoy, your brain releases a hormone called Dopamine. Dopamine can be released while running, painting, doing art projects or eating a great cupcake. Even something as simple as drinking water can cause the reward system to be activated. It is how we survive. This is how pleasurable habits are formed. When we do something that causes dopamine to be released and we are rewarded with a good feeling, we go back to that activity to achieve that feeling again.
How does all of this play into addiction? Some pleasurable habits can be good; running every day is good for the cardiovascular system, muscular system, and skeletal system. Negative and dangerous habits form in the same way. Some examples of bad habits are overeating, misusing medication or other substances or drinking too much alcohol.
For some, it starts as experimentation. A person may try a particular substance for the first time. In this example, consider the substance to be an opioid. The first time a person tries an opioid, the brain lets it in because it causes more dopamine to be released and the pleasure sensors in the brain are stimulated. With such a strong pleasure reward, the brain will crave more and more. Over time, previously pleasurable activities like exercise or good food become less appealing as the brain becomes rewired to demand the pleasure provided through the opioid.
Harvard School of Public Health tells us that “Addiction exerts a long and powerful influence on the brain that manifests in three distinct ways: craving for the object of addiction, loss of control over its use, and continuing involvement with it despite adverse consequences. (2011)
Your brain can recover. “Like other chronic diseases such as heart disease or asthma, treatment for drug addiction usually isn’t a cure. Nevertheless, addiction can be managed successfully. Treatment enables people to counteract addiction’s disruptive effects on their brain and behavior and regain control of their lives. (National Institueon Drug Abuse (NIDA, 2016)

There are many different types of treatment programs available. Treatment helps the individual detox from the opioid and manage the cravings. Many of them also teach coping skills and how to build strong social networks to help avoid relapse. As time goes on, the brain adapts to treatment, the urges are less prevalent, and the individual can begin again to enjoy other pleasurable activities in their lives.
Looking for more information on your brain and addiction? Check out these links:
https://www.health.harvard.edu/newsletter_article/how-addiction-hijacks-the-brain
Treatment Defined: Part 3
This is the third and last in the “Treatment Defined” series. The purpose of this series has been to help readers understand what types of treatment are available, define them, offer resource information and simplify the language of treatment overall.
Previously we have described individual and group counseling as well as outpatient services. Lastly, we are going to talk about inpatient services. In this series segment, we are going to offer information on
- Short term residential programs
- Long term residential programs, and
- Detox programs
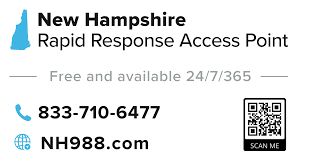
Please remember that one size does not fit all when it comes to treatment options. The inpatient resources described below may be a perfect fit for some but other individuals may find success in an outpatient setting might do better with outpatient. Please consult your doctor or call the NH Helpline to talk a clinician at 844-711-4357 or 211.
- Detoxification/Detox: Offered to assist an individual in the early stages of withdrawal from substance use, a detox program is a safe and monitored environment where trained health and social service professional can support individuals as they allow substances to filter out of their systems and manage the associated symptoms to minimize side effects.
- Short-term residential programs: An intensive, structured setting using a modified 12-step program. For this type of program, individuals usually spend 3-6 weeks in a hospital like setting before they begin outpatient therapy or self-help groups. The outpatient therapy portion is an important part of this program as it helps reduce the risk of relapse and helps the individual form new social bonds.

- Long-term residential programs: Offer care 24/7 in a non-hospital setting. Residence will vary between 6 and 12 months. These programs are generally very structured. Treatment in an environment of this type will rely on what is known as “social context” to help the individual identify ways to learn new, beneficial behaviors in a carefully while also learning to resist previous behaviors and unhealthy settings and relationships that might hinder recovery.
In this region, there are four (4) residential treatment options – three are located in Manchester. They are The Farnum Center, Cypress Center, and Westbridge Community Services (men only). In addition, Hampstead Hospital offers detox services in the region as well as other inpatient and outpatient services.
Please remember that one size does not fit all when it comes to treatment options. The inpatient resources below may be a perfect fit for some but other individuals may find success in an outpatient setting. Consider which option might meet your needs. Also, please consult your doctor or call the NH Helpline to talk a clinician at 844-711-4357 or 211 for additional information. .
Hampstead Hospital: http://www.hampsteadhospital.com/chemical_dependency.htm
Farnum Center: www.farnumcenter.org
Cypress Center: https://www.mhcgm.org/how-we-can-help/our-facilities/
Westbridge Community Services: https://www.westbridge.org/
Please look at the South Central Public Health Network Resource Guide for more information.
https://southcentralphn.org/wp-content/uploads/2018/06/SCPHN-Resource-Guide.pdf
Old Home Day – Safe Home Day

For over 100 years, Old Home Day has been observed in towns across NH as a way to celebrate the community and reconnect with friends and neighbors. Many towns in the Granite State celebrate Old Home Day with parades, barbeques, games, and fireworks. These events are well organized, well attended, and enjoyed by the young, old, and everyone in between. Let us all safely celebrate our towns in the great state of New Hampshire and ensure that good times, good food, and good company are the only things being reported in the news!
To keep you, your family, your friends, and neighbors safe during these joyous festivities, please follow these simple safety tips:
- When driving to your town’s Old Home Day, be aware of the increased number of pedestrians in the area. Slow down and observe traffic signals and crossing guards.

- When walking, cross the street only with a crossing guard, or at an intersection with a walk signal. If these are not available, walk at a crosswalk looking both ways: Left-Right-Left, then make eye contact with drivers as you cross.
 Put your phone down when walking (and driving) and be aware of
Put your phone down when walking (and driving) and be aware of
your surroundings (situational awareness).- Be mindful of choking hazards when collecting small giveaways from parades or booths.
- Use sunscreen and wear a hat. Parade routes are not typically in the shade.
- If you are attending celebrations at night, wear light colored clothing and or reflective gear. Carry a flashlight and use insect repellent for mosquitos. Give your children glow sticks to use at night – they are a fun way to make your child more visible. (You may find a good deal on glow sticks at a dollar store near you!)
- Drink plenty of water to stay hydrated and healthy.

- Carrying a little bottle of hand sanitizer or disinfectant wipes is always a good idea to keep your hands clean, especially before eating some of that delicious homemade fair food!
Old Home Day is also a great place for children to practice being independent, but only when parents feel that they are ready. Before heading over to the festivities remind children of the above safety tips and review the additional tips below:
- Phone Down-Heads up! Never walk while looking at your phone! Take your headphones out to hear the sounds of traffic.
- Stay in the celebration areas. Don’t wander away.
- Do not dart into the street or cross between parked cars.
- Walk on sidewalks or paths. If there are none, then walk facing traffic and as far to the left as possible.
- Drink water, not soda to stay hydrated and healthy.
Have your child watch this interactive presentation from Safe Kids Worldwide before going out.
Be safe, stay healthy, and enjoy celebrating your community with family, friends, and neighbors!